Osteoarthritis of the thumb
Osteoarthritis at the base of the thumb is very common in women over the age of 50. Occasionally arthritis can develop after fractures involving the base of the thumb. An examination of the wrist and thumb area together with x-rays will confirm the diagnosis.
Treatment will often involve initially rest and modification of activities or change of work practices. The use of simple pain killers or anti-inflammatory tablets is encouraged, often in conjunction with a splint. An intra-articular injection of steroid may also be given depending on the severity of the arthritic changes.
Treatment options
Surgery is used for disabling pain that cannot be controlled by other measures. There are several surgical procedures that can be used. The choice of which procedure is best for you depends upon the type of arthritis and your individual circumstances:

The metacarpal bone (at the base of the thumb) is divided and repositioned to reduce pain and improve use of the thumb for patients with mild/early arthritis.
The arthritic joint is removed and then two bones are fused together making one bone. This is most often performed in young and middle aged men who do manual work, and is thought to preserve the strength of the thumb better than other procedures.
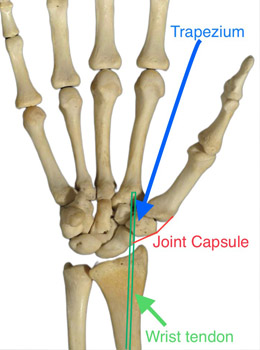
The trapezium (the small bone at the base of the thumb) is removed. It is sometimes necessary to stabilise the thumb by using a wrist/thumb tendon. Occasionally a pin is placed to temporarily “stabilise” the thumb base. This is the most common procedure performed in the UK for this type of arthritis.
Joint replacement
Mr Crook offers pioneering joint replacement surgery in the form of the Cartiva implant for base of thumb arthritis. Mr Crook is one of the Principal Investigators for the GRIP 2 study. He is one of only four UK surgeons involved in this prestigious International research trial in conjunction with highly regarded centres in the United States.
Traditionally the arthritic joint is replaced with either a Pyrocarbon or a Silicone joint. The long-term outcome of this operation is very variable. There are specific problems associated with these type of joint replacements such as loosening and dislocation. The Cartiva implant offers a possible solution to some of these problems. Additionally, other types of thumb replacement (which look very much like mini hip replacements) are available. Mr Crook will discuss the options with you in detail at your consultation.
The precise aftercare will depend upon the specific operation performed. The following specifically refers to Trapeziectomy.
You will normally be fit to go home soon after the operation, either the same day or the next day. The hand will be in a Plaster of Paris (POP). You will be prescribed painkillers to control the pain post-operatively.
The hand should be elevated as much as possible for the first 3-5 days to minimize swelling in the hand and fingers. The Plaster of Paris is worn for 7-10 days, after which a custom-made thermoplastic splint is applied by our Hand Therapist. The splint is kept for approximately 4-6 weeks.
Therapy exercises will commence to regain mobility and strength. Patients usually notice that the arthritic pain has gone within 8 weeks but the results improve between 6 and 12 months as the thumb strengthens.
Return to activities of daily living
Return to driving
You should not drive for at least 5 weeks following your operation. You need to be able to perform an emergency stop safely and use the gear stick, steering wheel and hand brake without difficulty. You should discuss the exact timing of returning to driving with your surgeon.
Return to work
This will depend on your individual working environment. Return to heavy manual labour should be prevented for approximately 8 weeks. Please ask your surgeon for advice.

